Dermatitis and Eczema: the various faces of skin diseases
The skin can be prone to various dermatitis and eczema, skin conditions that can take many different forms and can be caused by multiple causes.
DERMATITIS: UNDERSTANDING IT, TREATING IT, PREVENTING IT
The skin, the largest organ in the human body, is often exposed to numerous factors that can compromise its health and integrity. Among the most common conditions afflicting the skin is dermatitis, an umbrella term encompassing a variety of irritative and inflammatory skin manifestations. This condition, while not serious, can cause significant discomfort and negatively affect the quality of life of those affected.
The terms "dermatitis" and "eczema" are often used indiscriminately to describe skin inflammation. However, "dermatitis" generically means an inflammation of the skin, while "eczema" is a specific condition characterized by itching and redness.
WHAT IS DERMATITIS?
Dermatitis is an inflammation of the skin that occurs when the skin reacts to numerous stimuli, both internal and external. This reaction can be triggered by allergens, chemicals, physical factors such as heat or cold, or the internal release of inflammatory factors. Symptoms can vary considerably depending on the type of dermatitis, but generally include redness, intense itching, swelling and, in severe cases, scaling, blistering, blistering and skin erosion.
Although dermatitis is a common disorder, its impact should not be underestimated, as persistent forms can become complicated and a source of considerable physical and psychological distress. The condition is essentially noncontagious, but its manifestations can vary widely, often depending on triggers and individual predisposition.
The term "dermatitis" encompasses several skin conditions, most of which share the inflammatory symptoms described above.
Atopic Dermatitis (Atopic Eczema)
Atopic dermatitis, often called atopic eczema, is one of the most common forms and predominantly affects children but can persist into adulthood. This condition manifests as dry, itchy and cracked skin, often in skin folds such as the elbows, knees, neck, and other areas prone to moisture. The stages of this dermatitis alternate between periods of increased reactivity, with itchy, reddened rashes, and times of remission, where the skin may appear apparently healthy.
Causes include a combination of genetic factors, skin barrier alterations, and abnormal immune responses to common environmental allergens.
Seborrheic Dermatitis
Characterized by inflammation and scaling, seborrheic dermatitis occurs mainly on the scalp, face, ears, and areas rich in sebaceous glands. It is often associated with the presence of the fungus Malassezia with symptoms that may include red spots, itching and scaling, often confused with other conditions such as rosacea. Causes may include excessive sebum production and a genetic predisposition.
Contact Dermatitis
This form of dermatitis occurs when the skin comes into direct contact with allergens or irritants, causing an inflammatory reaction. Symptoms may include redness, itching, blistering, and sometimes crusting and scaling. This type of dermatitis is common in people who react to cosmetics, detergents, metals, or clothing. The inflammatory reaction is caused by activation of the immune system against these substances that are considered harmful.
Dermatitis Herpetiformis
Closely related to celiac disease, dermatitis herpetiformis manifests as an immune response to gluten. Patients develop itchy, bullous eruptions, mainly on the knees, elbows, and lumbar region. Although not all celiacs are affected, it is considered one of the main skin manifestations of gluten intolerance.
Perioral Dermatitis
Perioral dermatitis occurs around the mouth and sometimes extends to the cheeks, chin and forehead. The lesions resemble eczema or acne and can cause burning and itching. The exact cause is uncertain, but hormonal factors and certain substances in cosmetics and toothpastes are often implicated.
Sweat Dermatitis (Miliaria)
Also known as sudamine, sweat dermatitis is caused by blockage of sweat ducts, leading to a rash with small itchy blisters, typically in areas such as armpits, groin and body folds. It is more common in hot climates or during periods of intense physical activity. We can also bring into this category irritation from diapers, pads, and diapers, which occurs when the skin is in prolonged contact with moisture and irritants such as urine and feces. These conditions are more common in infants and the elderly with reduced mobility who use diapers.
SYMPTOMS AND SIGNS
The symptoms of dermatitis vary depending on the specific type and underlying causes, but they share some common features that can appear with varying intensity.
Among the most common symptoms:Reddening
- Itching
- Swelling
- Desquamation
- Blisters
- Bubbles
- Erosions
- Crusts
- Sensation of heat or burning
- Skin dryness
- Thickening of the skin (lichenification)
Typically, dermatitis manifests as a sudden inflammation of the skin accompanied by redness and swelling, followed by scaling and itching.
More severe forms may present with blisters, boils, and erosions of the skin that, if scratched or irritated further, lead to the formation of scabs.
Itching is one of the most persistent symptoms and can range from mild to intense. When itching is very severe, the person tends to scratch vigorously, which increases the risk of skin tearing and subsequent infection. In the affected areas, one may also feel a sensation of heat or burning that contributes to the overall discomfort.
The various forms of dermatitis or eczema can therefore have significant repercussions on daily well-being and, in severe cases, can even restrict movement in the affected areas due to pain or irritation. This symptom picture makes clear the importance of timely diagnosis and treatment to reduce discomfort and prevent complications.
DIAGNOSIS
The diagnosis of dermatitis or eczema is based on a methodical approach that begins with a detailed medical history. The dermatologist questions the patient about his or her personal and family medical history, including any episode of past illness, and gathers specific information about current symptoms and their course to identify possible causes or triggers, such as contact with known allergens or exposure to irritants.
A physical examination follows, during which the physician examines the skin lesions by observing the shape, size, pattern, and distribution of the eruptions and assesses for signs of infection or inflammation. Based on the results of this preliminary evaluation, one or more of the following tests may be prescribed:
- Skin scraping: to check for fungi that might mimic or complicate dermatitis.
- Skin swab: used to identify any bacterial or viral infections.
- Epicutaneous testing (patch test): to determine whether specific environmental allergens trigger dermatitis.
- Phototesting: performed if there is suspicion of an abnormal reaction to sunlight.
- Blood tests: including tests for total IgE, useful in cases of suspected atopic dermatitis, and thyroid function checks, relevant for some specific dermatitis.
PREVENTION
Preventing dermatitis completely may be impossible because the causes vary widely among different types. However, by adopting some general practices, it is possible to significantly reduce the risk of developing or exacerbating this skin condition:
- Nutrition: maintaining a balanced diet, rich in fruits and vegetables, is critical for skin health. These foods are rich in vitamins and antioxidants that can help maintain the integrity of the skin barrier. It is, in addition, helpful to include sources of omega-3 fatty acids, such as fish, known for their anti-inflammatory properties.
- Personal hygiene: it is essential to balance personal hygiene by using gentle cleansers that do not attack the skin. After bathing or showering, applying emollients and humectants such as glycerin or vegetable oils (e.g., almond oil) can help keep the skin moisturized and soft. It is important to avoid excessive washing, which can deprive the skin of natural protective oils. Also, avoid using harsh chemicals such as soaps, shower gels, and organic solvents that can cause unwanted skin reactions. For those working with potentially irritating substances, it is important to use personal protective equipment, such as suitable gloves, to protect the skin.
- Clothing: wearing clothing made of natural fibers such as cotton, which allows the skin to breathe, is recommended to reduce irritation. Fibers synthetic, on the other hand, can aggravate dermatitis by retaining heat and moisture.
- Use of emollients: applying emollients regularly can replace the use of soaps and help keep skin well moisturized. Emollients are especially useful after bathing and any time skin feels particularly dry or tight.
NATURAL TREATMENTS
In the treatment of dermatitis, in addition to traditional medical therapies, there are several natural alternatives that can help soothe symptoms and promote skin healing. These remedies are particularly valued for their gentleness and lower risk of side effects. Here are some of the most effective natural treatments for dermatitis:
- Aloe Vera: known for its soothing, cooling and anti-inflammatory properties, Aloe Vera is an excellent remedy for irritated and reddened skin. Aloe Vera creams offer immediate relief, while also helping to reduce inflammation and fight superficial bacterial infections.
- Calendula: the use of calendula creams is recommended to soothe itching and relieve skin irritation. This medicinal plant is renowned for its anti-inflammatory and healing properties.
- Zinc Oxide: often included in creams and ointments for skin treatment, zinc oxide is particularly useful for relieving irritation and itching. This mineral creates a protective barrier on the skin, promoting healing and preventing further damage.
- Rice Starch Bath: a lukewarm rice starch bath can be very beneficial to gently cleanse irritated skin and refresh it, while providing relief from irritation.
- Cold compresses: applying cold compresses to reddened and itchy areas can help reduce swelling and temporarily calm skin discomfort.
- Essential Oils: some essential oils, such as Lavender and Chamomile, are known for their calming properties and can be diluted in a neutral carrier cream (such as Sweet Almond oil) to treat affected areas locally.
- Plant and Herbal Extracts: a wide variety of plants possess anti-allergic and soothing properties, including Hypericum, Neem, Birch, Burdock, Violet, Fumaria, Helichrysum, Agrimony Eupatoria, and many others. These can be used in various forms, such as oils, creams or decoctions, for local applications or therapeutic baths.
These natural treatments, used individually or in combination, can offer valuable support in managing the symptoms of dermatitis, especially in mild to moderate forms. However, it is always advisable to consult a qualified dermatologist before starting any new treatment to ensure that it is safe and appropriate for your specific case of dermatitis.
MEDICAL TREATMENTS
Each type of dermatitis or eczema must be treated in a different, targeted manner. In fact, each treatment option is chosen based on the specific diagnosis, severity of symptoms, and the patient's individual response to treatment. It is essential to work with a dermatologist to determine the most effective and safe treatment regimen.
Alternatives include topical, physical, systemic, and biological therapies:
- Steroids: these drugs are effective in reducing inflammation and itching. They are applied directly to affected areas to control acute symptoms.
- Calcineurin inhibitors: these nonsteroidal agents are useful for treating inflammation without the risks of side effects typical of steroids, making them suitable for long-term use on sensitive areas such as the face and neck.
- JAK inhibitors: JAK (Janus Kinase) is an enzyme that transmits signals within cells, activating inflammatory processes. Relatively new to the therapeutic landscape, these topical drugs work by blocking specific inflammatory pathways, offering an alternative for more resistant cases.
- Phototherapy: controlled exposure to ultraviolet B or psoralen plus UVA (PUVA) treatments is often recommended for resistant forms of dermatitis, such as discoid eczema and chronic atopic dermatitis.
- Antihistamines: are used to relieve itching. Sedative antihistamines are especially effective at night to reduce scratching during sleep.
- Antibiotics and antivirals: if dermatitis is complicated by bacterial or viral infections, treatment may include specific antimicrobial agents.
- Immunosuppressants: for cases of chronic eczema that do not respond to standard treatments, immunosuppressive drugs may be prescribed to moderate the immune response
INTERACTIVE MEDICINE: NEXT-GENERATION PLANT-BASED TREATMENTS
In recent years, dermatological research has made significant strides in the treatment of sensitive skin. Alongside traditional remedies and medical treatments, new solutions based on the use of natural ingredients have been developed: this innovative approach, which we can call "interactive medication," aims not only to relieve symptoms but also to promote natural and lasting skin regeneration.
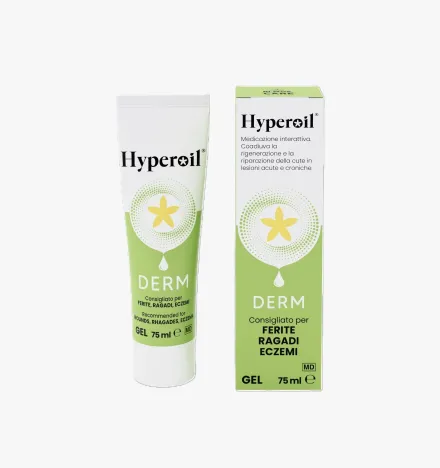
Among the therapeutic options available, we recommend products from the Hyperoil® line:
- Hyperoil® Gel Derm (GEL Vial 5ml): this gel, contained in convenient 5 ml vials, is ideal for treating small and medium-sized localized lesions. Key ingredients such as Neem Oil and Hypericum Oleolite offer healing and barrier properties, promoting tissue regeneration.
- Hyperoil® Gel Derm (75ml tube): for more extensive external injuries.
- Hyperoil® Oil (Vial 5ml): is indicated for deeper and more complex injuries, as it penetrates better into hard-to-reach tissues.
These interactive dressings, due to their ingredients derived from plants such as Neem and Hypericum, are designed to provide effective and natural treatment, reducing the need for more aggressive drug treatments. They combine the anti-inflammatory, antimicrobial and regenerative properties needed to effectively treat various types of dermatitis and eczema. Always consult a physician before starting a new treatment to ensure that it is the most suitable for your specific condition.
GENERAL TIPS FOR THE TREATMENT OF DERMATITIS AND ECZEMA
Managing dermatitis and eczema requires a careful and personalized approach to relieve symptoms and prevent flare-ups. Here are some general tips that can help:
- Skin hydration: applying emollient creams or ointments regularly helps keep the skin soft and moisturized. It is best to apply them immediately after bathing or showering to retain moisture.
- Identify and avoid substances that can irritate the skin: such as harsh detergents, perfumes, synthetic fabrics or wool. Using hypoallergenic and fragrance-free products can reduce irritation.
- Managing stress: which can aggravate the symptoms of dermatitis and eczema. Relaxation techniques such as meditation, yoga or simple breathing exercises can be helpful.
- Avoid scratching: it can worsen inflammation and increase the risk of infection. Keep nails short and, if necessary, wear cotton gloves at night.
- Adopt a balanced diet: consuming foods rich in vitamins and minerals supports skin health. Omega-3 fatty acids, found in fish, may have beneficial anti-inflammatory effects.
- Maintain a humidified environment: using a humidifier in the home can prevent dryness in the air, helping to keep the skin hydrated, especially in the winter months.
- Protect the skin: cold, wind and intense sun can irritate the skin. Apply appropriate protective cream and cover yourself with appropriate clothing when outdoors.
- Follow the doctor's instructions: it is important to follow the therapies prescribed by the dermatologist and report any changes in symptoms for effective treatment.
TIPS:Use gentle personal hygiene products: opt for nonaggressive soaps and cleansers such as PURO H® Foam, a plant-based cleansing mousse that removes impurities while respecting the skin's normal balance. This product is enriched with Hypericum Flower Oleolite, prebiotics and probiotics, making it suitable for even the most delicate and sensitive skin.
RELIEVES SYMPTOMS WITH PURO H® FOAM
Adopting these daily practices can significantly help improve the quality of life for those suffering from dermatitis and eczema. However, it is essential to consult a health care professional for a personalized treatment plan.
Products to treat Dermatitis
Do you have a question?
Our team of experts has an answer for you!
What is the difference between tissue regeneration and repair?
In case of injury, the physiological reflex of the organism and thus of the tissues is to evolve toward a regenerative and/or reparative process.
The difference between these two mechanisms is:
- Regeneration:
damaged tissues are replaced with cells of the same type. - Repair:
damaged tissues are replaced with connective tissue (fibrosis).
Why is the use of topical steroidal anti-inflammatory drugs (cortisone ointments) not recommended to treat an injury?
Steroidal anti-inflammatory drugs cause the scarring process to stop, torpid sores, promoting the development of bacterial and fungal infections.
Why is the use of disinfectants not recommended to treat an injury?
Disinfectants (based on iodine, chlorine, oxygen peroxide, etc.) are known to be histolesive. Used to ward off infection risks, they themselves become detrimental to tissue repair, being very potent inhibitors of cell proliferation, both of fibroblasts and keratinocytes.
The use of disinfectants, depending on the stage of the injury, causes these effects:
- re-initiation of the inflammatory process;
- pathological prolongation of the inflammatory phase;
- failure to progress to the granulation stage;
- stopping the granulation phase;
- inhibition of re-epithelialization;
- scar fibrotization (poor quality scarring).
What are the stages of wound healing?
There are three stages of wound healing:
- Stage 1: exudative or inflammatory or also called cleansing stage
- Stage 2: granulation or proliferative phase (granulation tissue formation)
- Stage 3: epithelialization or regenerative phase (scar formation and epithelialization)
What does "primary dressing" mean?
A primary dressing is one that is placed in direct contact with the injured tissues and interacts with the physiological processes of the injury.
What does "secondary dressing" mean?
A secondary dressing does not interact with the wound, but serves to:
- fill a cavity to absorb excess exudate and maintain the primary dressing over the wound;
- cover a wound to protect it while absorbing excess exudate and maintaining the primary dressing on the wound;
- Fix other secondary dressings and/or the primary dressing on the site of the injury.
Highlights
Choose the beneficial properties of our plant-based products to treat skin lesions and care for your skin.
Subscribe to our newsletter and get 10% off!
Stay up to date with the latest news, promotions, and exclusive offers from RI.MOS. CARE.