Knowing about Pressure Sores
Pressure sores, also known as pressure ulcers, are skin lesions that mostly affect people confined to bed or a wheelchair for prolonged periods. However, with the right treatment strategies, they can be prevented and managed effectively.
PRESSURE SORES: UNDERSTANDING THEM, TREATING THEM, PREVENTING THEM
Pressure sores, or pressure ulcers, are more or less severe injuries that develop on the skin and underlying tissues due to prolonged pressure in certain areas of the body. This problem occurs mainly in people who are bedridden for prolonged periods or have reduced mobility and can lead to very serious consequences if not properly treated. For this reason, it is essential to know how to prevent it, recognize it, and treat it appropriately.
They typically occur in areas of the body most exposed to constant pressure, such as the buttocks, heels, elbows, and lower back.
In these areas, reduced blood flow caused by prolonged pressure impairs tissue nourishment, leading to tissue necrosis and the formation of open ulcers.
WHAT ARE PRESSURE SORES?
Pressure sores are skin lesions caused by severe and prolonged pressure that can grow from small redness to deep wounds and cause major damage to underlying tissues.
This phenomenon is particularly common in elderly individuals, patients who cannot move independently, and people with conditions that limit the ability to move or impair blood circulation.
It is essential to understand that pressure sores are not common wounds: while superficial wounds can heal spontaneously, pressure sores tend to become chronic if not treated properly.
The stages of pressure sores
Pressure sores are classified into four stages, based on the severity of the injury:
- Stage I: the skin appears reddened and may have a sensation of heat, itching or discomfort. There are no open lesions yet, but inflammation is evident. The manifestation regresses if pressure is reduced in the affected skin area.
- Stage II: dermal destruction occurs with the appearance of a superficial lesion. The lesion may appear as an open blister or as an abrasion. The skin is damaged and a superficial ulcer begins to form.
- Stage III: the damage extends to the subcutaneous tissue and panniculus adiposus, with the presence of deeper ulcers. The lesion presents as an open cavity that may expose subcutaneous tissue but without involving muscle, tendon, or bone.
- Stage IV: this is the most severe stage, characterized by necrosis of muscle, periosteum, and possibly bone. The injury is deep and may involve muscles, tendons, and joints, with extensive tissue necrosis. Complications at this stage can include severe infection and osteomyelitis.
Causes
The causes of pressure sores are mainly attributable to prolonged immobility, forcing the person to maintain a fixed position, as is the case with fractures, severe obesity, or neurological diseases with motor impairment.
The absence of movement increases pressure on specific areas of the body, reducing blood flow and, in the long run, causing tissue death and pressure ulcer formation.
In addition to immobility, there are several other risk factors that contribute to the development of these injuries:
- Certain health conditions, such as diabetes and diseases that impair blood circulation, make the skin more vulnerable. In particular, obesity, which reduces blood flow to fatty tissues, and also excessive thinness, with exposed bone protrusions, increase the risk of injury.
- Malnutrition, incontinence, and fragile skin facilitate the occurrence of pressure sores, hindering tissue regeneration and increasing the risk of infection.
- Specific conditions that make patients particularly susceptible to pressure ulcers such as coma states, periods of postoperative convalescence, and neurodegenerative diseases such as amyotrophic lateral sclerosis, which drastically reduce a patient's mobility. Spinal cord injuries are also a significant risk factor.
- Environmental and physical factors, such as the use of excessively hard surfaces (e.g., inadequate mattresses or seats) or high body weight, contribute to aggravation.
SYMPTOMS AND SIGNS
The symptoms of pressure sores usually begin with a simple reddening of the skin, which does not disappear even after the pressure is removed. Other manifestations may be added to this, such as:
- the sensation of being hot or cold to the touch;
- slight swelling;
- appearance of blisters or small open wounds in the more advanced stages.
The sacral area, given its conformation and the frequent supine position in bedridden patients, is particularly prone to these lesions, partly because of the risk of contamination with urine or feces, which can promote their development. The heels and areas around the trochanters are other commonly affected areas.
In some cases, "subdominate" sores may be found in which deterioration spreads beneath the apparently intact superficial layers. In these cases, the skin appears sunken or floating to the touch, indicating underlying damage that requires immediate intervention.
Diagnosis
Decubitus injuries are diagnosed by careful observation of the skin, which allows them to be classified into four stages of severity.
- Stage I: persistent reddening of the skin that does not bleach on pressure.
- Stage II: appearance of blisters or open wounds with redness or irritation of the surrounding area.
- Stage III: deeper skin opening with damage to underlying tissues.
- Stage IV: extensive injury involving muscle, bone, and sometimes tendons and joints.
When ulcers do not heal, it may be necessary to search for possible infection by MRI imaging or analysis of a tissue fragment taken from the affected area.
PREVENTION
To prevent pressure sores from forming or worsening, one must first reduce pressure on at-risk areas, but there are also other effective preventive measures:
- Change positions at least every two to three hours to stimulate blood circulation and reduce pressure on sensitive areas such as the sacrum, heels and elbows.
- Keep the skin clean and moisturized, using specific products to protect and nourish the epidermis, thus preventing micro-lesions.
- Use specific preps such as pillows and antidecubitus mattresses designed to evenly distribute body weight and minimize pressure in at-risk areas.
- Ensure a balanced diet enriched with nutrients critical for skin health and tissue regeneration.
- Carry out a proper cleansing regimen, avoiding aggressive procedures that could damage the skin or cause further irritation.
It is essential that these practices be implemented with the cooperation of qualified health care professionals and, when possible, with the support of the patient's family members. Constant monitoring of the patient's condition and tailoring preventive measures to the patient's specific needs are crucial to preventing the occurrence of pressure sores and effectively managing risk.
NATURAL REMEDIES
To treat minor pressure sores, natural remedies can be an effective option, always to be used with medical advice. These products, intended for local rather than systemic use, include oleolites, protective pastes and absorbent powders. Combined with careful hygiene and a balanced diet, these remedies can promote the healing process.
Among the most important ingredients for the treatment of pressure sores are:
- Hypericum: Hypericum Oleolite, made from the extract of Hypericum perforatum in vegetable oil, is indicated for healing mild and medium sores. It has antiseptic and anti-inflammatory properties, thanks to hypericin (which reduces inflammation) and hyperforin (a natural antibiotic). However, Hypericum can cause photosensitivity, so it is advisable to cover the treated area with gauze to prevent pigmentation when exposed to light.
- Corn Starch and Zinc Oxide: These compounds absorb moisture, relieve itching and inflammation, and are especially good for combating chafing dermatitis in irritated areas.
- Rapeseed phytosterols: derived from Brassica napus seeds, phytosterols stimulate cell regeneration, improve skin membrane function, and reduce redness and flaking.
- Aloe Vera: Aloe Vera gel has soothing and cooling properties, providing immediate relief. Rich in polysaccharides and vitamins, it promotes cell regeneration and relieves pain.
- Provitamin B5: moisturizing and protective, it supports cell renewal and maintains skin elasticity, reducing inflammation.
- Avocado unsaponifiable: thanks to flavonoids, it has antioxidant, moisturizing and emollient action.
- Shea butter or liquid Jojoba wax: both known for their moisturizing, elasticizing and nourishing properties, they are ideal for protecting and softening the skin
Herbal formulations for pressure sores are generally fragrance-free to avoid irritation and allergies, making them odorless and suitable even for sensitive skin.
MEDICAL TREATMENTS
Pressure sores in more advanced stages, such as III and IV, require specific interventions and medical supervision to ensure effective treatment and reduce the risk of infection and complications.
These treatments include the use of advanced dressings, disinfectants, and healing ointments, as well as education of family members for ongoing support at home.
Here is what is possible:
- Cleaning and disinfection: wounds should be kept clean to reduce the risk of infection. Aqueous antiseptic solutions are used to disinfect affected areas before other dressings are applied.
- Application of ointments and healers: ointments with healing properties, applied directly to the sore, promote tissue regeneration. After application, the wound is covered with breathable gauze, which protects the area without hindering perspiration.
- Disinfectants: the use of modern antibacterial products such as silver nanocrystals helps maintain the balance of bacterial load on the wound, reducing the frequency of dressings and limiting the formation of necrosis and fibrin.
INTERACTIVE MEDICINE: NEXT-GENERATION PLANT-BASED TREATMENTS
In recent years, dermatological research has made significant strides in the treatment of sensitive skin. Alongside traditional remedies and medical treatments, new solutions based on the use of natural ingredients have been developed: this innovative approach, which we can call "interactive medication," aims not only to relieve symptoms but also to promote natural and lasting skin regeneration.
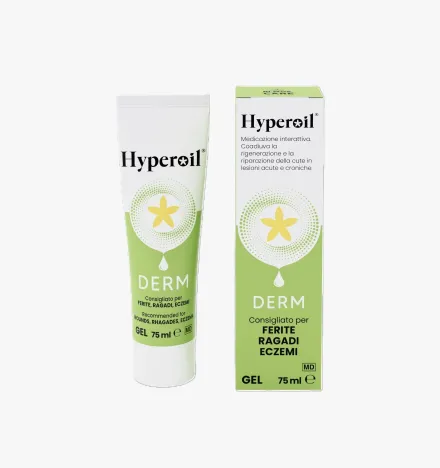
For pressure sores, the Hyperoil® OIL Spray (100 ml) and Hyperoil® GEL for complex lesions (75 ml) products from RI.MOS. CARE are ideal:
- Hyperoil® Oil Spray (100 ml): formulation with Neem and Hypericum provides effective protection, creating a barrier that promotes regeneration of damaged skin. Direct application to the sore helps keep it clean, reducing the formation of fibrin and necrosis and limiting the risk of infection.
- Hyperoil® GEL for complex lesions (75 ml): similar to the spray, this gel is formulated to assist tissue repair and healing, reducing erythema and inflammation in the treated area. It too contains Neem and Hypericum extracts, offering benefits in skin protection and regeneration.
These interactive dressings are indicated for complex injuries such as ulcers, pressure sores, hemorrhoids, and other wounds that require healing by second intention, often chronic or infected.
GENERAL TREATMENT ADVICE
To effectively manage pressure sores, one must be careful during treatments.
TIPS:First of all, it is recommended to have the patient change positions every 15 minutes to relieve pressure.
It is essential then:
- Inspect the skin daily, paying special attention to the most vulnerable areas, to identify early signs of inflammation or redness.
- Clean and dry the skin regularly, using pH-balanced products, keeping it hydrated at all times.
- Maintaining a balanced and nutritious diet, possibly consisting of light and frequent meals, is crucial to prevent any nutritional deficiencies that could aggravate the situation.
Regarding the use of Hyperoil® products, in case of self-medication, it is recommended to dress the ulcer once a day if infection is present, and every other day for noninfected lesions, isolating with cotton or TNT bandages.
In prevention, daily application of a small amount of Hyperoil® to areas at risk of injury is helpful. One should, however, avoid the use of patches, which can cause maceration, erythema, blisters or further skin injury.
Products to treat Pressure Sores
Do you have a question?
Our team of experts has an answer for you!
What is the difference between tissue regeneration and repair?
In case of injury, the physiological reflex of the organism and thus of the tissues is to evolve toward a regenerative and/or reparative process.
The difference between these two mechanisms is:
- Regeneration:
damaged tissues are replaced with cells of the same type. - Repair:
damaged tissues are replaced with connective tissue (fibrosis).
Why is the use of topical steroidal anti-inflammatory drugs (cortisone ointments) not recommended to treat an injury?
Steroidal anti-inflammatory drugs cause the scarring process to stop, torpid sores, promoting the development of bacterial and fungal infections.
Why is the use of disinfectants not recommended to treat an injury?
Disinfectants (based on iodine, chlorine, oxygen peroxide, etc.) are known to be histolesive. Used to ward off infection risks, they themselves become detrimental to tissue repair, being very potent inhibitors of cell proliferation, both of fibroblasts and keratinocytes.
The use of disinfectants, depending on the stage of the injury, causes these effects:
- re-initiation of the inflammatory process;
- pathological prolongation of the inflammatory phase;
- failure to progress to the granulation stage;
- stopping the granulation phase;
- inhibition of re-epithelialization;
- scar fibrotization (poor quality scarring).
What are the stages of wound healing?
There are three stages of wound healing:
- Stage 1: exudative or inflammatory or also called cleansing stage
- Stage 2: granulation or proliferative phase (granulation tissue formation)
- Stage 3: epithelialization or regenerative phase (scar formation and epithelialization)
What does "primary dressing" mean?
A primary dressing is one that is placed in direct contact with the injured tissues and interacts with the physiological processes of the injury.
What does "secondary dressing" mean?
A secondary dressing does not interact with the wound, but serves to:
- fill a cavity to absorb excess exudate and maintain the primary dressing over the wound;
- cover a wound to protect it while absorbing excess exudate and maintaining the primary dressing on the wound;
- Fix other secondary dressings and/or the primary dressing on the site of the injury.
Highlights
Choose the beneficial properties of our plant-based products to treat skin lesions and care for your skin.
Subscribe to our newsletter and get 10% off!
Stay up to date with the latest news, promotions, and exclusive offers from RI.MOS. CARE.