Getting to know Urticaria: symptoms, causes, and treatment strategies
Urticaria is a common skin condition that can cause significant discomfort. Knowing the symptoms, causes, and possible treatment strategies is essential to best deal with it.
URTICARIA: UNDERSTANDING IT, TREATING IT, PREVENTING IT
Urticaria manifests as a rash with red, itchy pomples. It is a common condition that can be transient or evolve into a chronic form and can be triggered by various factors.
Origin of the name Urticaria
The name "urticaria" originates from the Latin term Urtica, the botanical name for nettle, because of the symptoms similar to those caused by contact with this plant. The leaves of the nettle, release, in fact, an irritant substance that, upon contact with the skin, causes rashes, itching and a numbing sensation, due to interaction with the hair-like trichomes on the plant.
WHAT IS URTICARIA?
Urticaria manifests as a rash that may cover localized areas or extend over large areas of the body. This dermatologic condition is characterized by the presence of pomphi, which are raised skin lesions that are round or irregular in shape, varying in size and color from red to skin-like, accompanied by itching.
The onset of urticaria is typically triggered by an intense release of histamine and other chemicals from mast cells, which are vital cells of the immune system. This release induces an inflammatory reaction visible on the skin.
Although many episodes of acute urticaria do not require medical treatment and tend to recede on their own, the symptoms can be bothersome.
Depending on the duration of an attack, it is possible to speak of acute urticaria or chronic urticaria.
Types of urticaria
Urticaria is mainly distinguished into acute and chronic, depending on the duration of the episode.
- Acute urticaria: usually resolves within six weeks and accounts for about 70% of cases. It occurs rapidly, often peaking within 8 to 12 hours, then disappearing within one or two days. However, it can last longer as new pomphi can continue to form even when the previous ones have receded. Among the most common triggers of acute urticaria are food allergens, environmental agents, medications, insect stings, infections, emotional stress, and physical stimuli. Acute urticaria is usually mild, but can sometimes indicate a severe allergic reaction, such as anaphylaxis, requiring immediate medical attention.
- Chronic urticaria: persists for more than six weeks and has an often fluctuating course, with phases of remission and relapse. The causes may be autoimmune, that is, related to a reaction of the immune system against its own tissues. This form can occur in association with other diseases such as rheumatoid arthritis and systemic lupus erythematosus.
Inducible types include:
- Delayed pressure urticaria: appears after prolonged pressure on the skin, such as from lifting weights or tight clothing. The oozing and swelling may occur even several hours after the stimulus.
- Cold or heat urticaria: is triggered when the skin is exposed to temperatures that are too low or too high, causing erythema and rashes in the affected areas.
- Solar urticaria: triggered by exposure to sunlight, it can affect both sun-exposed and covered areas.
- Aquagenic urticaria: a very rare form in which even contact with water (such as rain or sweat) triggers a skin reaction.
- Contact urticaria: triggered by direct skin contact with specific substances or materials.
- Drug urticaria: arises in response to particular drugs that the body does not tolerate adequately.
- Viral urticaria: related to viral infections, such as those caused by certain viruses or parasites.
- Stress urticaria, which appears to be related to an altered emotional state, although there is no definitive scientific confirmation of the link between stress and the onset of urticaria.
Causes
Urticaria develops when the immune system responds to a stimulus by releasing histamine and other mediators of inflammation such as cytokines. These mediators cause local blood vessels to dilate, causing the characteristic skin swelling due to fluid leaking into the surrounding tissues, which resolves as the fluids are reabsorbed.
The causes of this phenomenon can be allergic or nonallergic in origin.
Major triggers include:
- Food allergens: such as nuts, shellfish, eggs.
- Respiratory infections: particularly common in children.
- Medications: such as antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs) and ACE inhibitors, which can cause angioedema through nonallergic mechanisms.
- Physical and environmental factors: such as exposure to extreme temperatures (cold or heat), sunlight, pressure on the skin (e.g., tight clothing), and strenuous exercise.
In adults, urticaria is often associated with an autoimmune response, as in chronic spontaneous urticaria, which can occur in people with autoimmune conditions, such as thyroiditis.
There are also factors that can worsen urticaria, including:
- Emotional stress
- Alcohol and caffeine
- Prolonged pressure on the skin
- Insect bites
- Exposure to extreme weather conditions
SYMPTOMS AND SIGNS
Urticaria is a dermatological condition known for its unpredictability and the variety of symptoms it can manifest. This skin condition is evidenced through:
- Pruriginous pomphi: raised skin lesions, often with a pale center and red edges. They can often change shape, size, and location rapidly.
- Intense itching: The pomphi are typically itchy, and the itching may intensify with exposure to heat or contact with irritants.
- Swelling: more or less significant in specific areas of the body, such as around the eyes, lips, and extremities, such as the hands and feet. This symptom is particularly important because it can signal the presence of angioedema, a deeper and potentially dangerous form of swelling.
Complications
One of the most serious complications of urticaria is angioedema, which occurs in a significant percentage of cases, in both acute and chronic forms. This condition involves more extensive swelling, affecting the deeper layers of the skin or even submucosal tissues, and can affect different parts of the body, including sensitive and visible areas such as the eyes and lips, as well as more extensive areas such as the genitals.
Symptoms of angioedema include:
- Pain and a burning sensation in the affected areas.
- Respiratory problems due to airway narrowing.
- Swelling of the conjunctiva, which can lead to obvious redness and ocular discomfort.
Given its potential severity, angioedema requires prompt medical intervention, especially if respiratory distress occurs, a symptom that can rapidly progress and require emergency treatment.
Diagnosis
To effectively treat urticaria, it is essential to understand what triggers it. This is done by gathering detailed information from the patient and, if necessary, by laboratory testing.
It is also important to distinguish urticaria from similar conditions that require different treatments, such as pemphigoid or vasculitis. If the urticaria is of recent onset or has persisted for some time, consulting a dermatologist is essential to get an accurate diagnosis and set up the right treatment.
PREVENTION
There are several ways to prevent urticaria: if it is allergic in origin, you should try to reduce or eliminate exposure to the triggering allergen. For other types of hives, it is helpful to identify them with the help of a dermatologist, who can give advice on how to avoid them so as to reduce the risk of new episodes.
NATURAL REMEDIES
For those looking for less invasive solutions to manage hives, there are several natural remedies that can offer relief from symptoms:
- Aloe vera: Topical application of aloe vera gel can provide significant relief from itching due to its soothing and cooling properties. The gel can be applied directly to lesions to relieve symptoms.
- Cold compresses: applying cold compresses can help reduce itching and inflammation. A towel or cloth soaked in cold water and applied to the affected area for a few minutes can be very effective.
- Baths with colloidal oatmeal: taking a bath with colloidal oatmeal can soothe irritated skin and calm inflammation. Oatmeal has natural soothing properties that are especially helpful for sensitive and irritated skin.
- Herbal infusions: drinking herbal infusions such as chamomile or green tea can help because of their anti-inflammatory properties. These teas can also be applied locally as cold compresses to reap direct benefits on the skin.
- Essential oils: essential oils of lemon balm, lavender, and chamomile are known for their calming properties and can be used in aromatherapy or diluted in a carrier oil and applied to the skin to relieve itching and irritation.
These natural remedies can be useful for managing mild urticaria or as an adjunct to traditional medical treatments but it is always recommended to consult a physician before starting any new treatment to ensure that it is safe and effective for your specific case.
MEDICAL TREATMENTS
Management of urticaria begins with identification and elimination of triggers, especially for inducible forms and drug reactions. However, most cases of urticaria resolve spontaneously without the need for specific treatments. When they are needed, treatments vary according to the form of urticaria, acute or chronic, but all aim primarily at symptom control, especially itching.
Commonly adopted drug treatments include:
- Antihistamines: these are the treatment of first choice for urticaria, both acute and chronic. Second-generation antihistamines are preferred because they cause less drowsiness than first-generation antihistamines.
- Corticosteroids: in severe cases of acute urticaria, or during acute outbreaks in chronic urticaria, oral corticosteroids may be prescribed for short periods to decrease inflammation.
- Immunosuppressants: in situations of chronic urticaria resistant to other treatments, immunomodulatory or immunosuppressive agents, such as cyclosporine, can be used; however, these can lead to an increased risk of side effects.
- Biologic drugs: for patients with chronic urticaria who do not respond to standard treatments,monoclonal antibodies that neutralize IgE are used.This is an approved option and has been shown to be effective in reducing the frequency of the pomphi and the intensity of itching.
INTERACTIVE MEDICINE: NEXT-GENERATION PLANT-BASED TREATMENTS
In recent years, dermatological research has made significant strides in the treatment of sensitive skin. Alongside traditional remedies and medical treatments, new solutions based on the use of natural ingredients have been developed: This innovative approach, which we can call "interactive medication," aims not only to relieve symptoms but also to promote natural and lasting skin regeneration.
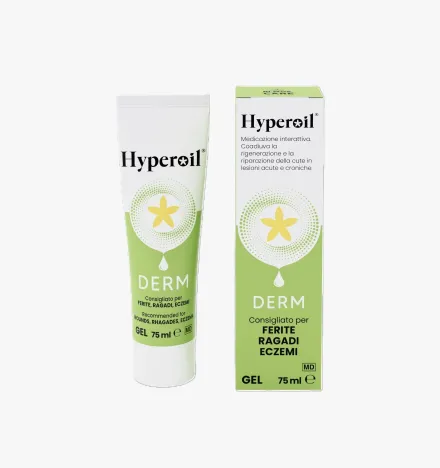
To relieve itching and skin irritation associated with urticaria, Hyperoil® Vial Derm Gel 5 ml may be an excellent option. This gel, enriched with Neem seed oil and Hypericum flower extract, is especially suitable for sensitive areas and can help calm inflammation and itching associated with urticaria while supporting the skin's healing process.
GENERAL TREATMENT ADVICE
Managing urticaria effectively requires a careful and personalized approach. Here are some general tips that can help control symptoms and improve quality of life:
- Maintaining a healthy lifestyle: a balanced diet, rich in antioxidants and low in processed foods and additives, can support the immune system and reduce inflammation. Regular exercise and adequate sleep are also essential for managing stress, a known aggravating factor in urticaria.
- Avoid scratching: it can aggravate irritation and increase the risk of infection.
- Wear comfortable clothes: soft and loose fabrics reduce friction on the skin.
- Hydration: drinking plenty of water helps keep the skin hydrated.
- Follow a balanced diet: it can strengthen the immune system and reduce allergic reactions.
To keep the skin clean and further soothe irritation, you can use PURO H® Foam, a gentle cleansing mousse. Suitable for all skin types, even the most sensitive, this mousse contains Hypericum flower oleolite and is enriched with prebiotics and probiotics, respecting the natural balance and helping to maintain the integrity of the skin barrier and prevent further irritation.
RELIEVES SYMPTOMS WITH PURE H FOAM
One must, however, always keep in mind that each case of urticaria may be unique, and what works for one person may not be effective for another. Working with a physician is crucial to finding the most appropriate and safe treatment strategy.
Products to treat Urticaria
Do you have a question?
Our team of experts has an answer for you!
What is the difference between tissue regeneration and repair?
In case of injury, the physiological reflex of the organism and thus of the tissues is to evolve toward a regenerative and/or reparative process.
The difference between these two mechanisms is:
- Regeneration:
damaged tissues are replaced with cells of the same type. - Repair:
damaged tissues are replaced with connective tissue (fibrosis).
Why is the use of topical steroidal anti-inflammatory drugs (cortisone ointments) not recommended to treat an injury?
Steroidal anti-inflammatory drugs cause the scarring process to stop, torpid sores, promoting the development of bacterial and fungal infections.
Why is the use of disinfectants not recommended to treat an injury?
Disinfectants (based on iodine, chlorine, oxygen peroxide, etc.) are known to be histolesive. Used to ward off infection risks, they themselves become detrimental to tissue repair, being very potent inhibitors of cell proliferation, both of fibroblasts and keratinocytes.
The use of disinfectants, depending on the stage of the injury, causes these effects:
- re-initiation of the inflammatory process;
- pathological prolongation of the inflammatory phase;
- failure to progress to the granulation stage;
- stopping the granulation phase;
- inhibition of re-epithelialization;
- scar fibrotization (poor quality scarring).
What are the stages of wound healing?
There are three stages of wound healing:
- Stage 1: exudative or inflammatory or also called cleansing stage
- Stage 2: granulation or proliferative phase (granulation tissue formation)
- Stage 3: epithelialization or regenerative phase (scar formation and epithelialization)
What does "primary dressing" mean?
A primary dressing is one that is placed in direct contact with the injured tissues and interacts with the physiological processes of the injury.
What does "secondary dressing" mean?
A secondary dressing does not interact with the wound, but serves to:
- fill a cavity to absorb excess exudate and maintain the primary dressing over the wound;
- cover a wound to protect it while absorbing excess exudate and maintaining the primary dressing on the wound;
- Fix other secondary dressings and/or the primary dressing on the site of the injury.
Highlights
Choose the beneficial properties of our plant-based products to treat skin lesions and care for your skin.
Subscribe to our newsletter and get 10% off!
Stay up to date with the latest news, promotions, and exclusive offers from RI.MOS. CARE.